Clinical profile of 28 cases of disorders of sexual development in a referral center
Main Article Content
Abstract
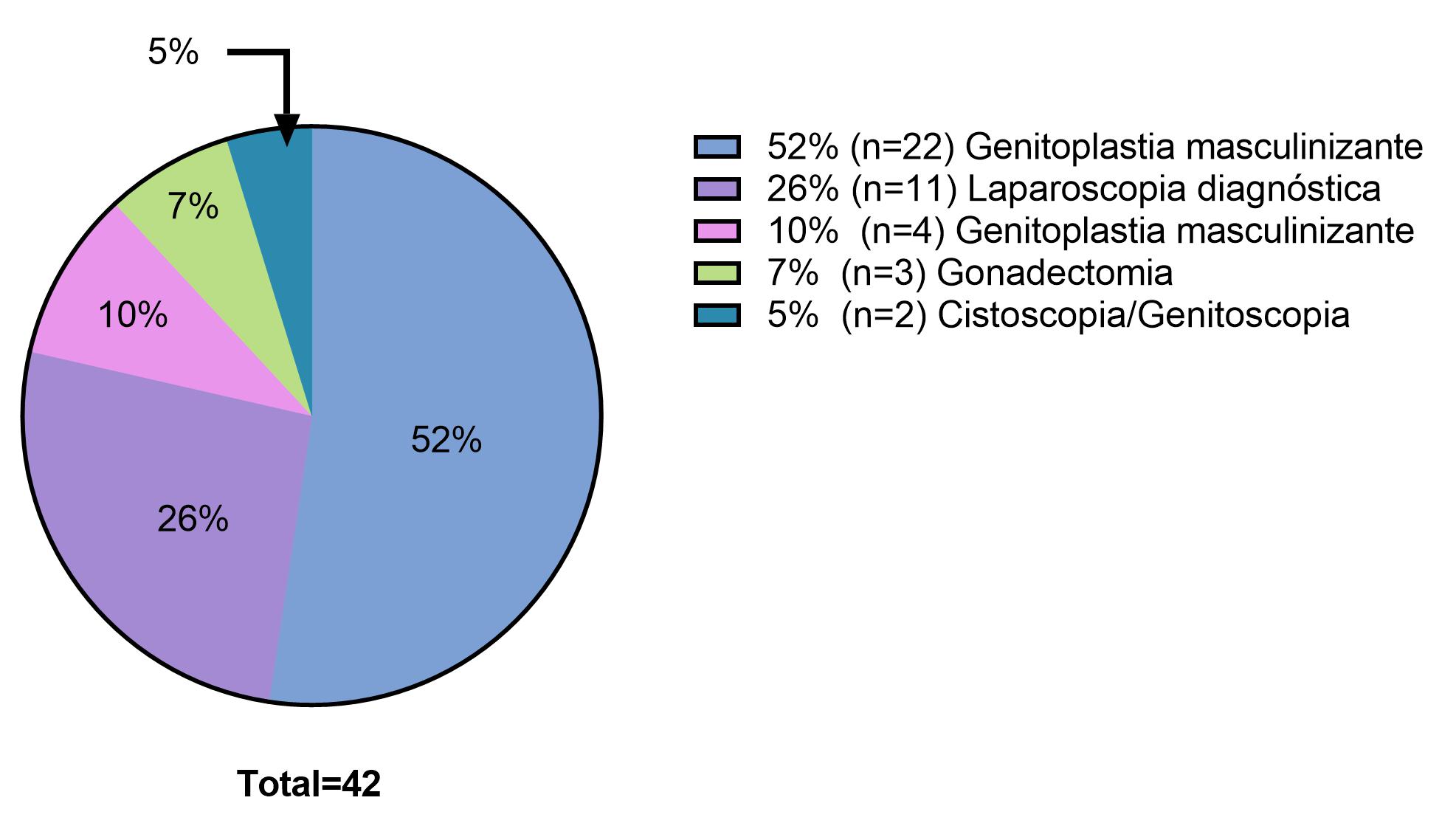
Background: Disorders of sexual development (DDS) include a group of rare clinical entities. The low prevalence of these diseases and their social impact on the community require the systematic registration of the clinical information of the patients. Objective: To characterize the clinical spectrum of cases of disorders of sexual development other than Turner and Klinefelter syndrome evaluated at the Hospital Universitario San Ignacio. Methods: for each case, an electronic form designed in the RedCap® tool was filled out, the variables considered for the registry were chosen following the recommendations of the International Registry of Sexual Differentiation Disorders (I-DSD). A total of 28 patients were included, 2 were diagnosed with a type of sex chromosome disorder, 17 were diagnosed with a 46, XY type of sexual development disorder and 9 with some type of 46, XX sexual development disorder. Different molecular tests were performed in 96.4% of cases, managing to define an etiological diagnosis in 7/28 of the cases. Conclusions: our findings highlight the importance of cytogenetic studies as first-line tests in the diagnostic approach of patients with DDS. This work is the beginning of the first registry of disorders of sexual development, not only institutional but also national, and will very surely provide academic bases for the construction and execution of future research that will generate evidence-based recommendations to improve the clinical care of individuals affected with some type of DDS.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Creative Commons
License Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
You are free to:
Share - copy and redistribute the material in any medium or format.
Adapt - remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms.
• Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
• NonCommercial — You may not use the material for commercial purposes.
• ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
• No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
References
Lee PA, Houk CP, Ahmed SF, Hughes IA, International Consensus Conference on Intersex organized by the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. Consensus Statement on Management of Intersex Disorders. PEDIATRICS 2006;118:e488–500. https://doi.org/10.1542/peds.2006-0738. DOI: https://doi.org/10.1542/peds.2006-0738
Thyen U, Lanz K, Holterhus PM, Hiort O. Epidemiology and initial management of ambiguous genitalia at birth in Germany. Hormone Research 2006;66(4):195–203. https://doi.org/10.1159/000094782. DOI: https://doi.org/10.1159/000094782
Mazen I, Hiort O, Bassiouny R, El Gammal M. Differential diagnosis of disorders of sex development in Egypt. Hormone Research 2008;70(2):118–23. https://doi.org/10.1159/000137657. DOI: https://doi.org/10.1159/000137657
Mota BC, Barros Oliveira LM, Lago R, Brito P, Canguçú-Campinho AK, Barroso U, et al. Clinical profile of 93 cases of 46, XY disorders of sexual development in a referral center. International Braz J Urol 2015;41(5):975–81. https://doi.org/10.1590/S1677-5538.IBJU.2014.0544. DOI: https://doi.org/10.1590/S1677-5538.IBJU.2014.0544
Fernández N, Moreno O, Rojas A, Céspedes C, Forero C, Mora L, et al. Manejo transdisciplinario de pacientes con desórdenes del desarrollo sexual en Colombia. Limitantes para un manejo oportuno e integral. Urología Colombiana 2017;26(3):164-168. https://doi.org/10.1016/j.uroco.2016.06.004. DOI: https://doi.org/10.1016/j.uroco.2016.06.004
Kolon TF. Disorders of Sexual Development. In: Philip M. Hanno SBM and AJW, editor. Penn Clinical Manual of Urology, Elsevier Inc.; 2007, p. 827–52. https://doi.org/https://doi.org/10.1016/B978-1-4160-3848-1.X1000-5. DOI: https://doi.org/10.1016/B978-141603848-1.10025-7
García Acero M, Moreno Niño O, Suárez-Obando F, Molina M, Manotas MC, Prieto JC, et al. Disorders of sex development: Genetic characterization of a patient cohort. Molecular Medicine Reports 2020;21(1):97–106. https://doi.org/10.3892/mmr.2019.10819. DOI: https://doi.org/10.3892/mmr.2019.10819
Berglund A, Johannsen TH, Stochholm K, Viuff MH, Fedder J, Main KM, et al. Morbidity, Mortality, and Socioeconomics in Females with 46,XY Disorders of Sex Development: A Nationwide Study. Journal of Clinical Endocrinology and Metabolism 2018;103(4):1418–28. https://doi.org/10.1210/jc.2017-01888. DOI: https://doi.org/10.1210/jc.2017-01888
Berglund A, Johannsen TH, Stochholm K, Aksglaede L, Fedder J, Viuff MH, et al. Incidence, prevalence, diagnostic delay, morbidity, mortality and socioeconomic status in males with 46,XX disorders of sex development: A nationwide study. Human Reproduction 2017;32(1):1751–60. https://doi.org/10.1093/humrep/dex210. DOI: https://doi.org/10.1093/humrep/dex210
Cox K, Bryce J, Jiang J, Rodie M, Sinnott R, Alkhawari M, et al. Novel associations in disorders of sex development: Findings from the I-DSD registry. Journal of Clinical Endocrinology and Metabolism 2014;99(2):E348-55. https://doi.org/10.1210/jc.2013-2918. DOI: https://doi.org/10.1210/jc.2013-2918
Röhle R, Gehrmann K, Szarras-Czapnik M, Claahsen-van der Grinten H, Pienkowski C, Bouvattier C, et al. Participation of adults with disorders/differences of sex development (DSD) in the clinical study dsd-LIFE: design, methodology, recruitment, data quality and study population. BMC Endocr Disord 2017;17:52. https://doi.org/doi: 10.1186/s12902-017-0198-y. DOI: https://doi.org/10.1186/s12902-017-0198-y
Aatsha, Krishan K. Embryology, Sexual Development. 2020.
García-Acero M, Moreno O, Suárez F, Rojas A. Disorders of Sexual Development: Current Status and Progress in the Diagnostic Approach. Current Urology 2019;13(4):169–78. https://doi.org/10.1159/000499274. DOI: https://doi.org/10.1159/000499274
Shawky RM, Elsayed NS, Ibrahim DS, Seifeldin NS. Profile of genetic disorders prevalent in northeast region of Cairo, Egypt. Egyptian Journal of Medical Human Genetics 2012;13(1):197–205. https://doi.org/10.1016/j.ejmhg.2011.10.002. DOI: https://doi.org/10.1016/j.ejmhg.2012.03.003
Berglund A, Viuff MH, Skakkebæk A, Chang S, Stochholm K, Gravholt CH. Changes in the cohort composition of turner syndrome and severe non-diagnosis of Klinefelter, 47,XXX and 47,XYY syndrome: a nationwide cohort study. Orphanet Journal of Rare Diseases 2019;14(1):16. https://doi.org/10.1186/s13023-018-0976-2. DOI: https://doi.org/10.1186/s13023-018-0976-2
Yu X, Nassar N, Mastroiacovo P, Canfield M, Groisman B, Bermejo-Sánchez E, et al. Hypospadias Prevalence and Trends in International Birth Defect Surveillance Systems, 1980–2010. European Urology 2019;76(4):482–90. https://doi.org/10.1016/j.eururo.2019.06.027. DOI: https://doi.org/10.1016/j.eururo.2019.06.027
Woud SG in t., van Rooij IALM, van Gelder MMHJ, Olney RS, Carmichael SL, Roeleveld N, et al. Differences in risk factors for second and third degree hypospadias in the national birth defects prevention study. Birth Defects Research Part A - Clinical and Molecular Teratology 2014;100:703–11. https://doi.org/10.1002/bdra.23296. DOI: https://doi.org/10.1002/bdra.23296
Catti M, Deméde D, Valmalle AF, Mure PY, Hameury F, Mouriquand P. Management of severe hypospadias. Indian Journal of Urology 2008;24(2):233–40. https://doi.org/10.4103/0970-1591.40621. DOI: https://doi.org/10.4103/0970-1591.40621
Witchel SF, A.Lee P. Ambiguos genitalia. Pediatric Encocrinology, Elsevier; 2014, p. 107–56. https://doi.org/https://doi.org/10.1016/B978-1-4557-4858-7.00014-7. DOI: https://doi.org/10.1016/B978-1-4557-4858-7.00014-7
Berglund A, Johannsen TH, Stochholm K, Viuff MH, Fedder J, Main KM, et al. Incidence, prevalence, diagnostic delay, and clinical presentation of female 46, XY disorders of sex development. Journal of Clinical Endocrinology and Metabolism 2016;101(12):4532–40. https://doi.org/10.1210/jc.2016-2248. DOI: https://doi.org/10.1210/jc.2016-2248
Arboleda VA, Vilain E. Yen & Jaffe’s Reproductive Endocrinology. 2014.
Acero MG, Moreno O, Gutiérrez A, Sánchez C, Cataño JG, Suárez-Obando F, et al. Novel homozygous mutation in a colombian patient with persistent mullerian duct syndrome: Expanded phenotype. International Braz J Urol 2019;45(5):1064–70. https://doi.org/10.1590/S1677-5538.IBJU.2018.0808. DOI: https://doi.org/10.1590/s1677-5538.ibju.2018.0808
Rane SR, Dangmali DP, Vishwasrao SD, Puranik SC. Persistent Mullerian Duct Syndrome with Testicular Seminoma in Transverse Testicular Ectopia. J Hum Reprod Sci 2018;11(3):300–2. DOI: https://doi.org/10.4103/jhrs.JHRS_54_18
Délot EC, Vilain EJ. Nonsyndromic 46,XX Testicular Disorders of Sex Development. GeneReviews® (Internet), 2015.
Anomalía del desarrollo sexual 46,XX ovotesticular. Orphanet Journal of Rare Diseases8 n.d. https://doi.org/10.1148/rg.326125507. DOI: https://doi.org/10.1148/rg.326125507
Swartz JM, Ciarlo R, Guo MH, Abrha A, Weaver B, DIamond DA, et al. A 46,XX Ovotesticular Disorder of Sex Development Likely Caused by a Steroidogenic Factor-1 (NR5A1) Variant. Hormone Research in Paediatrics 2017;87(3):191–5. https://doi.org/10.1159/000452888. DOI: https://doi.org/10.1159/000452888
Dalili S, Rad A, Kohmanaee S. Pure gonadal dysgenesis (46 XX type) with a familial pattern. Advanced Biomedical Research 2015;4:162. https://doi.org/10.4103/2277-9175.162536. DOI: https://doi.org/10.4103/2277-9175.162536
De Andrade JGR, De Angelo Andrade LAL, Guerra-Junior G, Maciel-Guerra AT. 45,X/46,XY ovotesticular disorder of sex development revisited: undifferentiated gonadal tissue may be mistaken as ovarian tissue. Journal of Pediatric Endocrinology and Metabolism 2017;30(8):1–6. https://doi.org/10.1515/jpem-2017-0039. DOI: https://doi.org/10.1515/jpem-2017-0039
Kalantari H, Asia S, Totonchi M, Vazirinasab H, Mansouri Z, Zarei Moradi S, et al. Delineating the association between isodicentric chromosome y and infertility: A retrospective study. Fertility and Sterility 2014;101(4):1091-6. ttps://doi.org/10.1016/j.fertnstert.2013.12.048. DOI: https://doi.org/10.1016/j.fertnstert.2013.12.048
Lehmann KJ, Kovac JR, Xu J, Fischer MA. Isodicentric Yq mosaicism presenting as infertility and maturation arrest without altered SRY and AZF regions. Journal of Assisted Reproduction and Genetics 2012;29(9):939–42. https://doi.org/10.1007/s10815-012-9822-y. DOI: https://doi.org/10.1007/s10815-012-9822-y
Miyado M, Muroya K, Katsumi M, Saito K, Kon M, Fukami M. Somatically acquired isodicentric y and mosaic loss of chromosome y in a boy with hypospadias. Cytogenetic and Genome Research 2018; 154(3):122-125. https://doi.org/10.1159/000488162. DOI: https://doi.org/10.1159/000488162